Advertisement
Research aims to better understand the tumor immune micorenvironment
Although the vast majority of patients with human papillomavirus (HPV)-associated oropharyngeal squamous cell carcinoma (OPSCC) can be cured with standard therapy, recurrence is often fatal. Research from Cleveland Clinic has identified immunologic factors that are associated with recurrence in a cohort of patients with recurrent/metastatic oropharyngeal cancer treated at a single institution and using data from The Cancer Genome Atlas (TCGA) database. The study, “Association of Suppressive Myeloid Cell Enrichment with Aggressive Oropharynx Squamous Cell Carcinoma,” appears in Cancers.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Prior research on tumor-infiltrating immune cells in head and neck cancer has indicated differences between HPV+ and HPV-negative patients. Patients with HPV+ OPSCC often have an improved clinical prognosis compared to patients with HPV-negative OPSCC. Tumor-infiltrating T lymphocytes such as CD8+ T cells, for example, have been associated with a more favorable prognosis for patients with HPV+ OPSCC. In contrast, tumor-associated macrophages (myeloid lineage cells) can be pro-inflammatory and immunosuppressive, and they have been associated with more advanced-stage disease, increased tumor invasiveness and increased tumor aggression. The authors of this retrospective case-control study note that their primary objective was to assess whether patients with clinically aggressive (recurrent/metastatic) OPSCC have a distinct immunosuppressive immune signature in the primary tumor.
“We used RNA expression profiling of pre-treatment surgical biopsies to examine the immunologic and gene expression profiles for patients who have known recurrence,” says Natalie Silver, MD, Director, Head and Neck Cancer Research in the Department of Otolaryngology-Head and Neck Surgery at Cleveland Clinic and senior author of the study. “It’s important to investigate the immune landscape for HPV+ patients who develop recurrence and metastasis in order to identify factors that contribute to worse clinical outcomes. We believe that having a better understanding of this can help guide and develop therapies for these patients and improve outcomes.”
The study included 37 pre-treatment tissue samples from HPV+ and HPV-negative OPSCC patients. The samples were organized into a case group (patients with known disease recurrence) and a control group (patients without disease recurrence). The patients had been treated at a single-center site between 2011 and 2019.
“We used banked formalin-fixed paraffin-embedded (FFPE) tumor tissue, and we focused our specimen selection to capture HPV+ patients with recurrence,” explains Dr. Silver. “Based on institutional numbers and survival rates, we were able to identify 20 patients with HPV+ OPSCC recurrent disease with adequate follow up and tissue for analysis.”
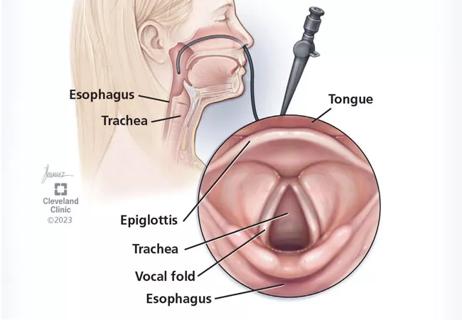
The research group defined recurrence as local and/or regional disease recurrence and/or distant failure after primary definitive therapy. Based on this definition, the four groups included in the study were HPV+ patients with recurrence (HPV+R+; n = 14), HPV+ patients without recurrence (HPV+R-; n = 12), HPV-negative patients with recurrence (HPV-R+; n = 5) and HPV-negative patients without recurrence (HPV-R-; n = 6). Of the patients, 81% were male and 26 (70%) had HPV+ cancer. Most patients were also current or former smokers. The primary subsite was the tonsil (n = 27) followed by the tongue base (n = 10).
Clinical data for all patient specimens were collected, and the samples were processed for analysis. An mRNA-expression immune-pathway profiling and analysis was performed.
The authors found that of the clinical data, gender, smoking status, subsite, N status and treatment were not associated with recurrence (P > .05). The group found that advanced T stage was the only clinical factor associated with recurrence in our cohort (95% CI, 0–0.9, P = .035).
In the HPV+R+ cohort, the disease-free survival rate as 10.8 months, and all patients from the study died of the disease (overall survival = 27.5 months). A total of 25% of patients had local recurrence, 25% had loco-regional recurrence and distant metastasis, and 50% had distant metastasis. Distant metastatic sites were the lung (which was the most common), followed by bone and brain.
Advertisement
A total of 32 patients had acceptable sequencing results which were analyzed by the research group. The fold-change expression of phenotypic markers for various immune cell populations was plotted using pheatmap.
“We observed a clustering of increased gene expression in both the myeloid cell and T cell populations in the HPV+R+ patients,” explains Dr. Silver. “However, GSEA [gene set enrichment analysis ] of HPV+R+ compared with HPV+R- patients showed significant enrichment of granulocytic-myeloid pathways, monocyte and megakaryocyte pathways. Additionally, T cell pathways were not significantly altered in HPV+R+ patients.”
Dr. Silver also notes that suppressive monocytes were significantly enriched in HPV+R+ patients (P = .004, family-wise error rate [FWER] P-value = .039) when compared to HPV + R- patients. However, GSEA analysis indicated significant enrichment of suppressive monocytes in the HPV-negative patients when compared to HPV+ patients (nominal P-value < 0.001, FWER P-value = 0.014).
“We examined individual gene expression data in the monocyte/macrophage pathway in the HPV+ R+ group and compared it to the HPV+ R- group,” says Dr. Silver. “We found increased fold change in several genes associated with poor differentiation of monocytes/macrophages.
Advertisement
The authors also performed GSEA pathway analysis on expression data from the head-and-neck-cancer TCGA database. The database included 499 patients, and 64 of them were recorded as HPV+. The researchers found that HPV-negative patients had increased suppressive monocyte/macrophage pathway enrichment (nominal P-value = .002, FWER P-value = .014) when compared to HPV+ patients. The researchers organized the patients into monocyte “hi” versus “low” groups based on their median expression and found no difference in survival according to the presence of monocyte/macrophage cells. Granulocytes (specifically neutrophilic metamyelocytes) were also enriched in HPV+R+ compared to HPV+R- patients.
“Our results show significantly increased gene enrichment in the suppressive monocytic/macrophage cell pathway and granulocyte cell pathway in patients with HPV+ recurrent disease and HPV-negative disease (in the institutional cohort), and in HPV-negative patients when compared to HPV+ patients (in the TCGA cohort),” explains Dr. Silver. “Since patients with recurrent HPV+ cancer have a more aggressive disease that clinically resembles more closely the HPV-negative patients, the finding of upregulation of the suppressive immune cell pathways in both of these cohorts may be an important factor associated with overall worse clinical outcomes and yield prognostic value.”
Dr. Silver notes that future work should focus on the effectiveness of monocytes/TAMs as a therapeutic target in more aggressive diseases, such as OPSCC patients with HPV+ disease with recurrence and HPV-negative HNSCC patients.
At the 2024 Combined Otolaryngology Spring Meetings, Dr. Silver presented research during the “Advances in Immunotherapy in Head and Neck Cancer” American Head and Neck Society session. She gave a talk titled “Immunogenicity and efficacy of an E6/E7-targeted prophylactic mRNA lipid nanoparticle vaccine for oropharynx cancer,” which expounds on the findings from the Cancers research.
Advertisement
The group developed a patented RNA lipid nanoparticle vaccine platform (RNA-LP) that unlocks antigen-specific T cell immunity by reprogramming the systemic and tumor immune microenvironment, specifically reprogramming the suppressive myeloid cell compartment. In the study, mice were given four weekly doses of E6/E7 mRNA-LP vaccine formulations before they were implanted with MEERL cancer cells (a model representing HPV-positive head and neck cancer). Twenty days after implantation, there was a significant reduction in MEERL tumor growth in the mRNA-LP vaccine-treated mice compared to the control mice. Furthermore, antigen-specific E6/E7 positive T cells were found after vaccine administration.
“These findings demonstrate initial immunogenicity, efficacy and antigen specificity of a prophylactic cancer vaccine for HPV-associated cancers,” says Dr. Silver. “More research is still needed to determine the response in a clinical group, but we believe that eventually this targeted vaccine may be used as prophylaxis for cancer recurrence after salvage surgery or definitive therapy in high-risk HPV-positive OPSCC patients.”
Advertisement
Advertisement

A new single-port system well-suited for oropharyngeal cancer treatment

Recommendations look to change mindset with CI referrals

Research could help direct care pathways for patients with unexplained swallowing difficulties

Strong communication with the patient and a thorough approach are essential
Cleveland Clinic physicians weigh in
New research adds to understanding of an understudied link
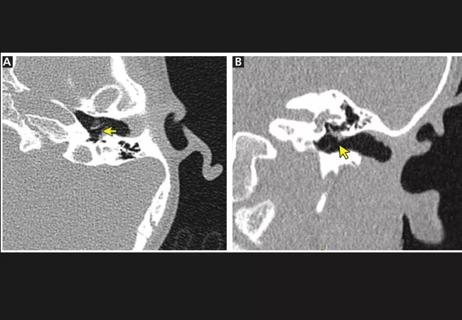
The rare condition can cause structural damage if untreated

A recently published case series highlights the broad range of laryngeal findings that can present among individuals with EDS